Payment integrity
Let’s partner your way to address your unique payment integrity challenges
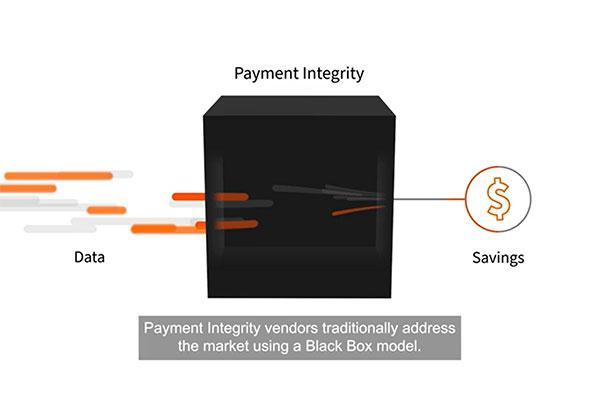
At EXL Health, we believe in a modular approach to payment integrity, allowing our customers to access vendor software, analytics, people, and processes to transparently identify and address overpayments, trends, and unique business challenges. Our innovative approach provides payers deeper insights into their payment integrity program through transparent and accessible information. Whether looking for a traditional solution or components within a modular delivery model, we partner with our clients to help make healthcare transformation happen.
Who we serve
EXL Health partners with and delivers our payment integrity services to both health plan payer and provider organizations. We support driving value-based outcomes and transformation in order to ensure payment accuracy and reduce fraud, waste, and abuse.
EXL Health is a proud to partner to:
- 7 of top 10 US Payers
- 2 of the top 3 PBMs
What we do
EXL Health’s Payment Integrity Services provide payers actionable insights at every touchpoint along the payment continuum to support comprehensive reimbursement initiatives and outcomes, including controlling costs, reducing overall health claim expenditure, optimizing revenue opportunities, and improving provider experiences.
Pre-pay & Post-pay Audit Solutions
We innovate by leveraging proprietary analytics technologies, best-in-class clinical reviews, and unparalleled expertise to mitigate over payments and maximize savings.
- Clinical claims auditing
- Inpatient, outpatient
- Ancillary
- Pharmacy auditing and analytics
- Third-party liability/subrogation services
- Pre-emptive solutions (E&M, provider education)
- Audit workflow
Payment Analytics & Data Mining
Through sophisticated data modeling, we apply our deep domain knowledge to find more and better savings.
- Provider billing analysis
- Provider abrasion analysis
- Provider intervention & education insights selection analytics
- Contract compliance
- Coordination of benefits (COB) reviews and eligibility related errors
- Subrogation workflow management software – MY SOCRATESTM
Payment Capacity Services
Our expert team provides deep domain knowledge and flexible support to execute your payment integrity needs, quickly and efficiently.
- Coding review
- Claims audit
- Appeal management
- Special investigation unit
Digital Transformation Services
Leveraging our multi-payer dataset and aggressively apply digital solutions, such as Artificial Intelligence (AI), natural language processing (NLP) and robotics processing automation (RPA), we maximize performance and financial-related results.
- Payment policy management
- Digitally enabled PI operations
- Selection analytics expertise
- Data science expertise
- Audit workflow management software
Proven outcomes: human ingenuity at work
One of our long-standing payer clients was looking to streamline their payment integrity program, specifically their Diagnosis-Related Group (DRG) auditing solutions. As their most trusted and first-pass post-pay vendor for DRG coding and clinical auditing services, they approached EXL when looking to reduce vendors to decrease administrative and operational workloads within vendor management. Leveraging human ingenuity, technology, and analytics-enabled solutions, EXL’s payment integrity solution was able to impact payment accuracies, cost management, and quality outcomes – all key to value-based performance success.
By partnering with our client to better understand their needs and implement custom solutions, EXL Health was able to create significant value to the organization, yielding an improved savings rate of 120% within 2020 and 2021.
- 30% overall DRG savings for client in 2020
- 56% overall DRG savings for client in 2021
- Expected continued growth in 2022
- Improved resource efficiency due to streamlining from a singular vendor