How EXL helped a large U.S. healthcare payer improve its Medicare sales
Introduction
This large US-based national healthcare payer had set goals to improve its Medicare sales and was looking for a way to aggregate and analyze its data to get better insights of overall lead generation and their sales performance. It chose to work with EXL as its single partner to bring all of its data sources to drive centralized Medicare Sales Reporting, and to drive sophisticated business insights and actions.
Challenge
Medicare Advantage market that provides great opportunity of growth for health plans, also comes with strong competition, with so many players struggling to retain existing members and enroll new members. To achieve success in this highly competitive market, where every Medicare beneficiary has multiple options to choose from, it is important for health plans to take smart data-driven informed decisions to guide them before, during, and even after the Annual Enrollment Period (AEP).
In generating such business-critical actionable insights, plans face challenges like either not having enough data, or inability to manage volumes of data coming from disparate sources. In this case, the payer’s existing framework had membership, call center, and product data all coming in from separate sources, making monitoring the sales performance for specific insurance products difficult. The payer identified challenges in running its teams’ performance reviews and had no visual dashboards to report on data and track enrollment performance.
The payer was unable to track its cost conversion rates within its marketing function, and also unable to link this to its sales goals. It wanted to identify targets for the highest commission channels, and look at historic estimates for different call center campaigns to compare their performance.
Solution
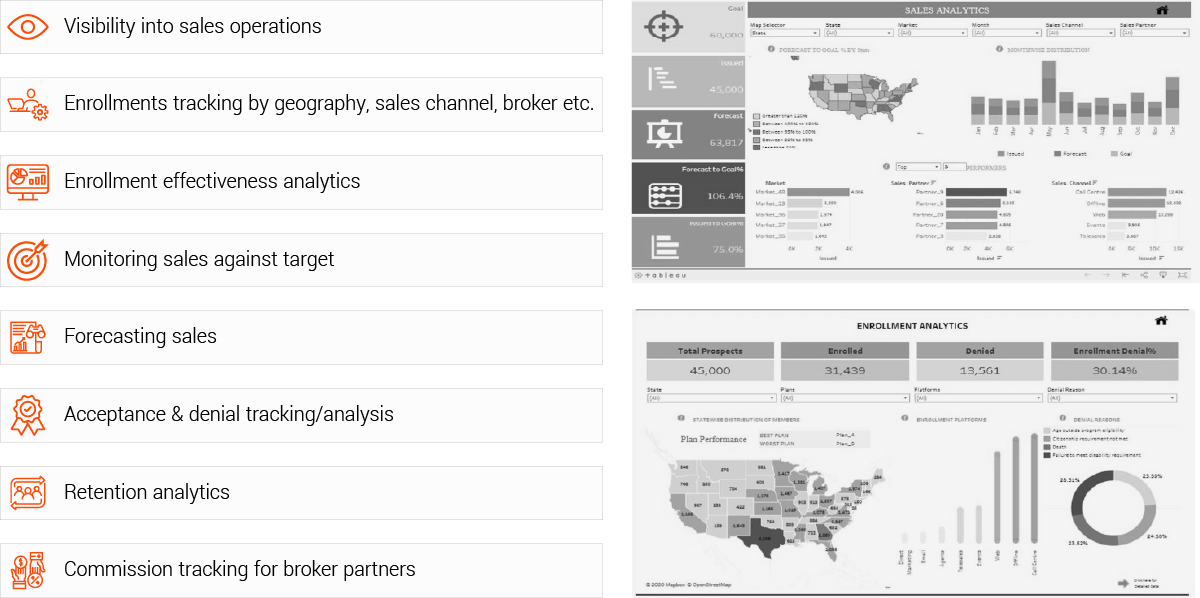
EXL Health has developed an analyticsdriven Medicare Sales performance solution, that helps health plans to optimize tracking and monitoring of their Medicare sales performance, which can be customized based on plan’s needs. For this payer, EXL’s solution empowered health plan leaders with persona-based dashboards to monitor call center performance, lead generation, sales conversion, member engagement and member retention with objective of growing their Medicare business and amplifying plan’s Medicare sales.
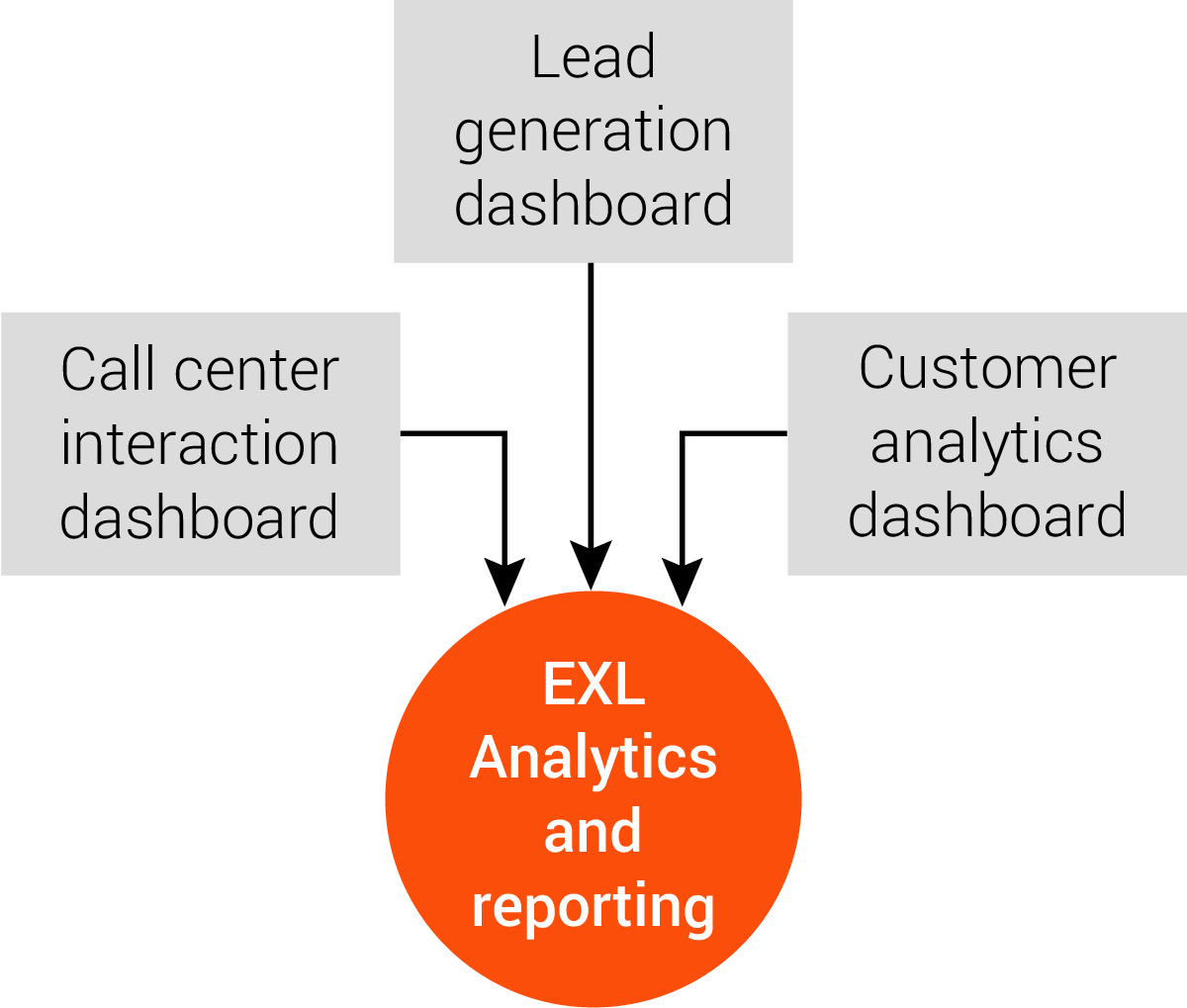
For this payer, EXL started by building three different dashboards:
- The call center interaction dashboard, designed to help monitor call center performance and bring efficiency to operations.
- The lead generation dashboard, to help monitor monthly allocations and make tactical adjustments as per performance to reach the target.
- The sales analytics and retention dashboard, to help analyze customer data and deliver insights regarding retention, cross-sell, and plan-related requirements.
The team built and linked these dashboards to an optimal funding model, which is used to identify the optimal funding for each campaign and the corresponding minimum cost of acquisition.
A further optimization model was created to identify maximum enrollments based on a given budget. With the new models, the payer can assess performance, choose the desired scenario, and allocate funds to the most cost-effective vendors on a monthly basis.
EXL also produced new models to assess the specific sales performance of each agent against their own specific selling criteria, allowing the payer to determine sales conversion by different media channels, agents, and geographical locations.
Outcomes
The dashboards quickly demonstrated several operational efficiencies and financial performance improvements including:
Lead generation: Brought down cost of acquisition by 25% during the AEP
Tactical adjustment with the best agent mapped with the best campaigns, helping the business increase conversion rate by two basis points
Helped the business reduce attrition by four basis points in six months, identifying customers who are highly likely to attrite as well as bring in extra leads with cross-sell opportunities
EXL’s approach was executed quickly, creating a centralized command center platform, at a lower cost than competitive offerings. The unified database has given the payer a speed-to-market advantage, with optimized use of data as a significant market differentiator.
